The April 29 summit was a high-profile opportunity to showcase for the medical field some of Merrimack’s great leaps in providing healthcare training for students, said School of Health Sciences Dean Kyle McInnis.
“I could feel a general excitement when I announced the new programs, including nursing, and the new nursing and clinical education center on campus,” McInnis said. “I think it really helped us get the word out.”
Merrimack created its School of Health Sciences two years ago offering undergraduate and graduate degrees. The school is enrolling its first nursing cohort in the fall and has over 700 applicants, McInnis said.
“They are the best and brightest we could find in the region and nationally,” he said.
The college broke ground on a 24,000-square-foot nursing school facility on May 1.
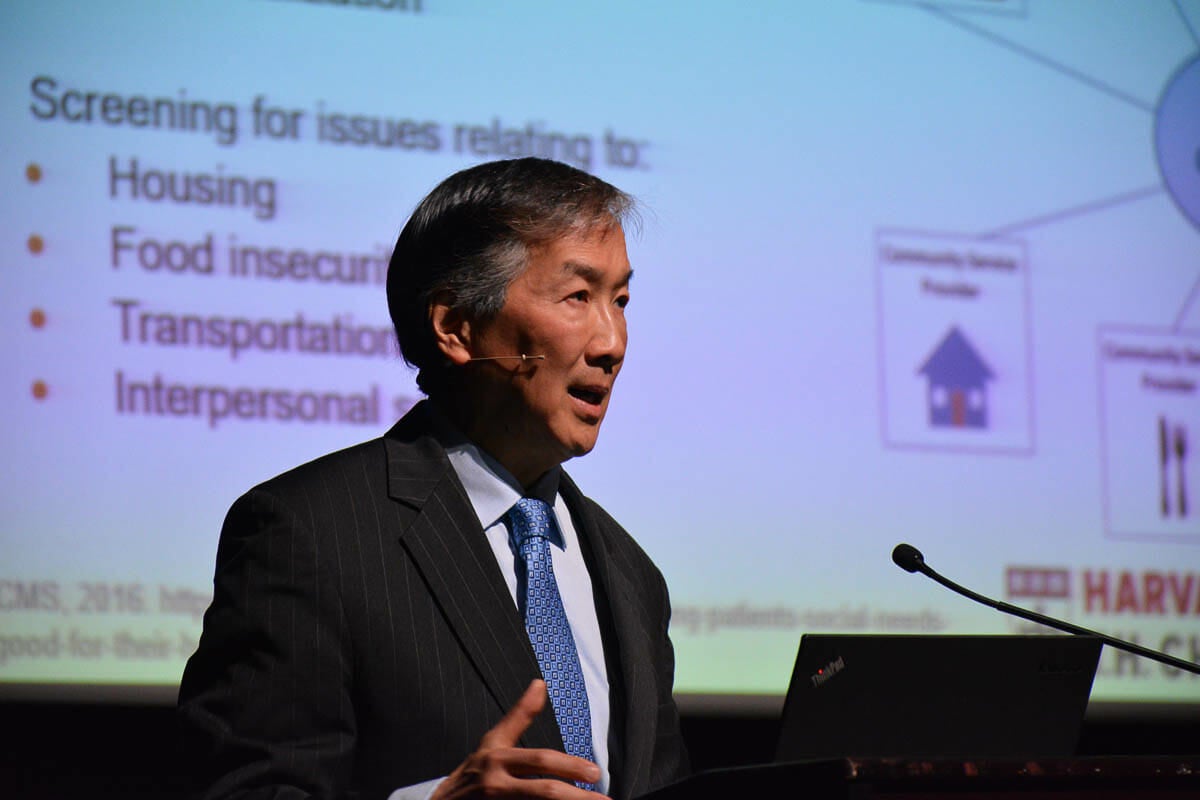
Dr. Howard Koh H’99, opened the half-day seminar as the keynote speaker discussing how there are many societal root factors for the quality of health and healthcare Americans experience. Improving societal determinants will improve healthcare, he said.
“Even if the contribution is small, we should be trying to move the needle on social determinants,” Koh said.
Equity and diversity are what social determinants of health is all about, he said. The United States has an increasingly diverse population by race and ethnicity. It will have a majority minority society by 2025. The challenge to healthcare providers is how to to care for everyone in such a diverse population that is also aging, Koh said.
Koh was assistant U.S. secretary for health under President Barack Obama; and previous to that was commissioner of public health for Massachusetts, appointed by then-Gov. Bill Weld. He is now Harvey V. Fineberg professor of practice of public health leadership at Harvard University’s Chan School of Public Health.
“There are a lot of challenges in healthcare and public health around the country,” he said.
Public health is anything that helps a person reach their highest attainable standard of health, Koh said. Increasingly, the medical field is interested in societal factors that go into public health such as where people live,their occupations, the quality of their education, quality of healthcare available to them and their ability to access it, even to the point of having mass transit to reach medical appointments.
“Social determinants are where you live, labor, learn, play and pray,” Koh said.
The life expectancy in the United States has declined for three straight years for the first time since 1993. Where Americans live plays a role in their life expectancy. A resident of Hawaii is expected to live to 81 years old but a resident of Mississippi only has a life expectancy to 78 years.
Societal factors cited by Koh included tobacco usage, high body mass index, and drug and alcohol usage.
He pointed out that as many as 4 million people miss or delay medical care, in part because they are aged or infirmed and can’t drive, they live in a rural area, or climate change prevents them.
“Health and transportation leaders should really be able to work together in the future if we’re really serious about healthcare,” Koh said.
The healthcare industry needs to work more closely with the free market which makes products that are unhealthy, he said. Already, great improvements are being made.
“Every business is a health business,” Koh said. Then he cited the auto industry which is making cars and trucks safer than ever with Volvo vowing to produce death-proof cars by 2020 and General Motors publicly claiming it also wants to create no-death vehicles with the added benefit of no emissions.
CVS Pharmacy rebranded itself CVS Health in 2014 and announced it no longer sells tobacco products and its revenues rose. Many pharmacies now give flu shots which is both good for health and a revenue producer.
Studies show that even attendance at religious or spiritual events leads to a 7-year increase in life expectancy. Medicaid it increasingly interested in social determinants, as well, Koh said.
“We start the conversation with leadership summits like this,” Koh said.
Other speakers included Dr. Davida Schiff, a general academic pediatrician and health services researcher; Vilma Martinez-Dominguez, the community development director for Lawrence, Mass.; and Dr. Robert Sege, of Tufts University School of Medicine, who is nationally recognized for developing approaches to health systems for preventing child abuse and neglect by improving support to families.
A grant from the Robert Wood Johnson Foundation helped fund the summit.